Disclaimer: This is not a sample of our professional work. The paper has been produced by a student. You can view samples of our work here. Opinions, suggestions, recommendations and results in this piece are those of the author and should not be taken as our company views.
Type of Academic Paper – Reflective Report
Academic Subject – Nursing
Word Count – 1342 words
The assignment provides an overview and insights into the experience with a patient and how it has resulted in the learning process. It also discusses the areas of improvement and actions that need to be taken to avoid any uncertain situations in the future for any such cases.
Being a radiotherapy student on placement, I was supposed to have a radiotherapy pre-treatment chat session with cancer diagnosed patients. Like any other patient coming for a CT scan before radiotherapy, to whom I had to give a first-day chat, I had to think about who the patient could be, what would be their level of perception and how I had to express myself. It was a challenge to stay prepared for any consequences and how adequately I should react to the possible situations.
I introduced myself then began the patient’s identification following the department protocol. Any examination or treatment regime in radiotherapy is unique to the individual. Therefore, the patient needs to be identified before any treatment procedure (The Royal College of Radiologists et al., 2008). When I started explaining the process and reason for a CT scan, I realized the patient showed unawareness about their radiotherapy cancer treatment and was also emotionally unsettled. He said nobody informed him of having radiotherapy treatment. After being diagnosed with cancer and recommended radiotherapy for the treatment, this is probably the first point of contact a patient has with the radiotherapy department. Therefore, it was important for me to create a trust to make the patient feel more comfortable and reassured; for the diagnosis of cancer would be as a shock to individuals who would exercise fear, anxiety, feel frightened, and would show natural reactions of uncertainty about tomorrow (Macmillan Cancer Support, 2017).
However, I made a sign to my supervisor, who came and took the time to listen to the patient who could still not remember much after the diagnosis. He then recalled to the patient the meeting they had with the consultant and radiotherapy recommended for treating their disease then instructed me to continue with the explanation of the CT scan process, after which we did the scan. With the patient reacting absurdly, I felt unsure of what I should do and say, but I felt a little relaxed after my supervisor came and handled the situation. After the scan took place, I went to my supervisor, showing my concern, upon which he reassured me that all information is computed to the patient, but they sometimes are unable to retain it for different reasons.
Before having this first-day chat, I was very confident, having done many first-day chats. I was surprised by the reaction, for it was the first time to have had such a challenging moment. I was also unsure about responding and did not feel experienced enough to deal with the situation alone. However, I was cautious with any verbal and non-verbal signs I showed because it was very important to communicate with the patient as first impressions effectively have a significant impact on further communication (Skills You Need, 2014). Although I was surprised, I could still understand why some patients may easily forget about the information they receive when informed of their cancer diagnosis but not a CT scan schedule. I could not also understand immediately how a patient would come for an appointment without being informed of the reason, especially for a radiotherapy pre-treatment CT scan.
My anxiety increased more when my supervisor joined us, wondering if he would decide to remain silent and ask me to continue the conversation, which I struggled to intervene in at that moment. I should have acted quickly and in the same way as my supervisor to deal with the situation effectively. The patient may feel that no interest is given to them personally, resulting in them lacking confidence in their treatment and care (Ramlaul and Vosper, 2013). Looking back, this experience had good and bad elements which have led to an increased understanding of my role within the radiotherapy team. I had to give more attention, evaluate the situation, and provide more explanation. However, I feel that I did not accomplish the task (O’Daniel and Rosenstein, 2008).
Orders completed by our expert writers are
From this experience, I am currently more aware of the significance of being self-assured and demonstrating professional skills in practice if a similar situation occurs in the future and not feel just as if I cannot accomplish something because of my position or experience. The understanding I have gained from this experience implies that I am presently more mindful of the implications of acting quickly and the significance of acting in the patient’s best interest. Nevertheless, a detailed study of similar cases and how patients react in different settings would have helped in a better understanding.
Most patients feel alarmed when informed of cancer diagnosis, which may bring huge nervousness and impact their daily lives, posing healthcare difficulties. This point is further supported by findings by Williams et al. (2017), identifying that an absence of information about radiotherapy procedures can increase the anxiety patients may experience at the commencement of treatment. Despite these difficulties, one of the imperative tools that will give a chance to understand more about this disease to provide quality healthcare is communication. On the other hand, communication can be challenging to healthcare professionals and patients, but if it is effective, patient satisfaction will be enhanced, resulting in superior cancer care (McCaffrey, 2011, p.121). What I could have done better was to have gone through some literature on dealing with possible situations and examining some cases that have taken place in the past.
Therefore, it was imperative to know and consider such frequently occurring incidents so they could be managed in a much better way. Insights of patients’ reactions and cases on how differently they may react in different situations would have helped me handle this case better. This is a fact that practically experiencing such cases would add to the learning and knowledge, but a theoretical understanding of previous cases would have still assisted. To improve for the next time, I would gather ample insights into how and where things may lead to and what effective measures could be adopted.
The assignment has focused on the learning outcomes of the particular scenario that is being faced. It has further inculcated the lags and inefficiency and the measures that need to be taken to avoid any such circumstances. It is learned that a prior review of the past cases may assist in avoiding any uncertain circumstances.
Institute for Healthcare Communication (2014). Impact of Communication in Healthcare. Available from: https://healthcarecomm.org/about-us/impact-of-communication-in-healthcare/. [Accessed 18 November 2017].
Macmillan Cancer Support (2017) Cancer and your feelings – Information and support. Available from: https://www.macmillan.org.uk/cancer-information-and-support/treatment/coping-with-treatment/cancer-and-your-emotions. [Accessed 15 November 2017].
McCaffrey RG. (2011). An educational program to promote positive communication and collaboration between nurses and medical staff. J Nurses Staff Dev.121-127.
National Cancer Institute (2014) Communication in Cancer Care. Available from: https://www.cancer.gov/about-cancer/coping/adjusting-to-cancer/communication-pdq. [Accessed 18 November 2017]
O’Daniel, M. and Rosenstein, A., H. (2008) Professional Communication and Team Collaboration. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2637. [Accessed on 18 November 2017].
Ramlaul, A. and Vosper, V. (2013) Patient-Centered Care in Medical Imaging and Radiotherapy. E-Book. revised. Elsevier Health Sciences, ISBN 0702055239, 9780702055232
SkillsYouNeed (2014) what is communication. Available from: https://www.skillsyouneed.com/ips/what-is-communication.html. [Accessed1 December 2017].
The Royal College of Radiologists, Society and College of Radiographers, Institute of Physics and Engineering in Medicine, British Institute of Radiology and National Patient Safety Agency (2008) Towards safer Radiotherapy. Available from: https://www.rcr.ac.uk/publication/towards-safer-radiotherapy. [Accessed 27 October 2017].
Williams, K., Blencowe, J., Ind, M., and Willis, D. (2017). Meeting radiation therapy patients’ informational needs through educational videos augmented by 3D visualization software. Journal of Medical Radiation Sciences, 64(1), 35–40. [Accessed 20 November 2017].
If you are the original writer of this Reflective Report and no longer wish to have it published on the www.ResearchProspect.com then please:
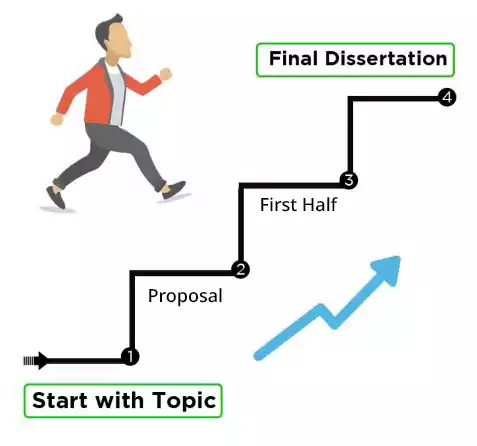
To prepare a master’s reflective report: